First proposed by Einstein in 1917
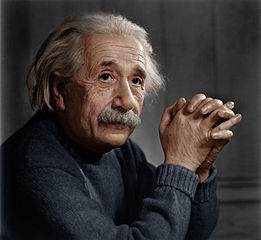 (L)ight (A)mplification by the (S)timulated (E)mission of (R)adiation was originally proposed by Albert Einstein (pictured right) in 1917. However, it was not until 1960 that the first, visible, laser light was produced by Maimen, using a ruby crystal; in 1966, a ruby laser was used in canine bladders by Parsons and, two years later, Mulvany attempted to fragment urinary calculi with a similar laser.
(L)ight (A)mplification by the (S)timulated (E)mission of (R)adiation was originally proposed by Albert Einstein (pictured right) in 1917. However, it was not until 1960 that the first, visible, laser light was produced by Maimen, using a ruby crystal; in 1966, a ruby laser was used in canine bladders by Parsons and, two years later, Mulvany attempted to fragment urinary calculi with a similar laser.
Laser physics
Einstein showed that light travels as small packets of energy (photons) and that most atoms exist naturally in a low-energy ("ground") state. By adding energy in the form of electricity, heat or light, atoms can be elevated to a higher energy ("excited") state so that they release a photon and then return to their ground state. So, when a photon strikes an excited atom, an additional photon is released of identical frequency & phase to the first, and the struck atom returns to its ground state. Photons within a lasing medium are reflected by semi-opaque mirrors so that they collide with excited atoms, releasing identical photons which, in cascade, collide with other excited atoms; the resulting photons are then combined to generate a laser beam (see video animation below) which exits through a non-opaque aperture in one of the mirrors.
How laser light is generated
The mechanism by which light is produced by a laser means, therefore, that the light is:
- coherent - the photons are all in phase,
- collimated - the photons all travel parallel with no divergence, and
- monochromatic - the photons all have the same wavelength (or colour, if within the visible spectrrum)
Different lasing media emit photons of different wavelengths which, combined with the power output and mode of emission (pulsed, continuous or Q-switched), determine the unique characteristics of any individual laser. Tissue properties (density, opacity, water content & blood flow) and wavelength govern how tissues respond to laser light. In general, longer wavelengths result in deeper tissue penetration and greater energy absorption by water.
Urological laser usage

- Soft tissue incision (e.g. urethral strictures, posterior urethral valves, endopyelotomy, bladder neck stenosis) - Holmium:YAG (Ho:YAG pictured right), Neodymium:YAG (Nd:YAG) or Potassium titanyl phosphate (KTP)
- Resection & ablation (e.g. benign prostatic hypertrophy, bladder tumours, condylomata, penile cancer, bladder cancer, skin haemangiomas) - Nd:YAG, Ho:YAG, Thulium:YAG (Thu:YAG), KTP, semiconductor diode or carbon dioxide (CO2)
- Lithotripsy (e.g. renal, ureteric & bladder stones) - Ho:YAG, pulsed dye or alexandrite
- Tissue welding (e.g. vasectomy reversal, hypospadias repair, strictures, fistulae, pyeloplasty, bladder augmentation, continent urinary diversion) - diode, KTP, Nd:YAG, CO2
- Autofluorescence (e.g. diagnosis of occult bladder cancer) - nitrogen laser
- Laser hair removal (e.g. on urethral grafts) - ruby, alexandrite, diode or Nd:YAG
The future
There is a huge amount of ongoing research in laser physics. It seems likely that new lasing media will allow the production of laser light across a wide wavelength which can then be tuned for tissue specificity. Plastic, conjugated polymers are amongst the most interesting lasing media under study, which could result in finely-tunable, cost-effective lasers, packaged in ultra-compact devices.
← Back to Lasers