What should I do if I have a testicular lump?
If you find a lump inside the scrotum, not arising from the skin of the scrotum itself, you should contact your GP immediately for further advice
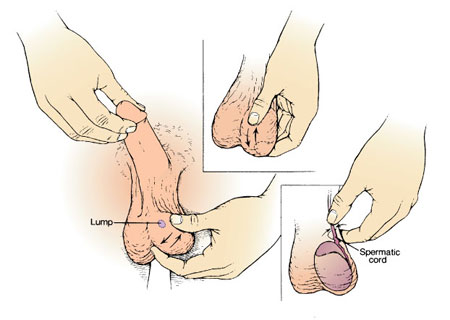
To feel for testicular lumps, it is best to examine yourself when you are warm and relaxed (e.g. after a bath or shower). Stand in front of a mirror and hold each testicle in turn between your fingers. Feel the body of the testicle and all the structures attached to it.
Download an information sheet on testicular self-examination
If your GP is concerned that you could have testicular cancer, you may be referred urgently to the urology department using the fast-track (2-week wait) referral system.
What are the facts about testicular lumps?
- The vast majority of swellings in the scrotum are benign and should not give cause for concern;
- Benign swellings in the scrotum only require surgical treatment if they cause significant symptoms (e.g. aching, cosmetic embarrassment);
- A simple ultrasound scan will usually differentiate between benign and cancerous swellings;
- If the lump is attached to the surface of the testicle, it is probably benign;
- If a lump is within the body of the testis itself, there is a 90% chance that it is a testicular cancer;
- Testicular cancer is the commonest malignant tumour in men between 20 and 50 years old;
- Whilst testicular cancer is rare in men over the age of 50, certain forms do occur and you should always seek advice from your GP;
- Testicular cancer is commoner in abnormal testicles e.g. previously undescended testicles, testicles which have been injured or infected and soft, atrophic testicles (sometimes seen in infertile men); and
- Early diagnosis and treatment mean that more than 95% of men can be cured of testicular cancer, even if it has spread beyond the testicle itself.
What should I expect when I visit my GP?
Your GP should work through a recommended scheme of assessment for patients with a scrotal swelling. This will normally include some or all of the following:
A full history
Your GP will take a full history, paying particular attention to any possible trauma or infection of the testicles in the past. You should mention any previous operations on your testicles to your GP, especially surgery for an undescended testicle. Please tell your GP if you have had a vasectomy in the past.
A physical examination
A full physical examination will be performed, including examination of your scrotum, your abdomen and your lymph glands. Your blood pressure will normally be measured as part of this examination.
Additional tests
a. General blood tests
The actual tests performed will be left to your GP's discretion. It is common to measure kidney function & liver function, and to check the blood cells for anaemia or other problems.
b. Tumour markers
 If your GP suspects testicular cancer, he/she may arrange some specific blood tests to measure tumour markers (alpha-fetoprotein, beta-human chorionic gonadotrophin, lactate dehydrogenase).
If your GP suspects testicular cancer, he/she may arrange some specific blood tests to measure tumour markers (alpha-fetoprotein, beta-human chorionic gonadotrophin, lactate dehydrogenase).
c. Other specific tests
An ultrasound scan (pictured, showing a testicular tumour) will normally be arranged to assess exactly where the swelling is in relation to your testicle. Depending on the findings of the ultrasound scan, a CT scan of your abdomen & chest may also be arranged. This is normally fixed through the urology unit.
What could have caused my testicular lump?
Swellings of the scrotum are usually cystic (fluid-filled), inflammatory or solid. Clinical examination and ultrasound scanning can usually differentiate between the possible causes
Cystic (fluid-filled) swellings
 These are the commonest swellings and are usually caused by a hydrocele (fluid around the testicle, pictured), a cyst in the epididymis (sperm-carrying mechanism) or varicose veins above the testicle (a varicocele). They are all benign and only require treatment if they cause significant symptoms.
These are the commonest swellings and are usually caused by a hydrocele (fluid around the testicle, pictured), a cyst in the epididymis (sperm-carrying mechanism) or varicose veins above the testicle (a varicocele). They are all benign and only require treatment if they cause significant symptoms.
Inflammatory swellings
Infection of the epididymis (sexually-acquired or secondary to a urinary infection), twisting of the testicle (torsion, usually in children) or infection of the testicle itself (e.g. due to mumps) are the commonest causes of inflammation.
Solid swellings
Solid swellings include tuberculosis & syphilis (both very rare nowadays), a sperm granuloma or nodule (usually following a previous vasectomy), chronic inflammation of the epididymis. If the lump is within the testicle itself, it may be a testicular tumour.
Information about chronic epididymitis
Hernias
A hernia arising in the groin can extend down towards the testicle but simple examination will reveal that the swelling does not arise from the scrotum itself. Urologists do not treat hernias and your GP may recommend referral to a hernia surgeon.
What treatments are available for this problem?
Cystic (fluid-filled) swellings
Hydrocele repair, excision of an epididymal cyst (pictured) and open surgery, laparoscopic surgery or radiological embolisation may be needed for significant symptoms from the swelling. Otherwise, no treatment is necessary.
Download leaflets on hydrocele repair or on excision of an epididymal cyst
Download leaflets on varicocele treatment by open surgery, keyhole (laparoscopic) surgery or radiological embolisation
Inflammatory swellings
Antibiotics are used for infection of the epididymis. Your GP may refer you to a urologist (if you are over 50 or have a urinary infection) or to a genitomedical clinic (if you are young or your infection may be sexually-acquired). Testicular involvement with mumps usually requires no specific treatment apart from painkillers. Suspected torsion of the testis requires emergency admission and immediate surgery.
Information about treatment of torsion of the testis
Testicular cancer
If you are found to have testicular cancer, you will be referred urgently to the urology clinic. Following further investigations (see above), you will normally be advised to have the testicle removed as soon as possible. An artificial testicle can be inserted at the same time or at a later date.
Removal of the testicle for cancer
Insertion of an artificial testicle
The need for further treatment (radiotherapy or chemotherapy) is determined by the pathology results, the results of your tumour marker blood tests & the findings on a CT scan. Once surgery has been arranged, you will referred to an oncologist for any further treatment and for long-term follow-up.
Other solid swellings
Tuberculosis and syphilis are rarely seen nowadays but are treated with appropriate antibiotics. Sperm granulomas in the epididymis may be removed if they are uncomfortable but they do not always require treatment.
Removal of the epididymis
Page dated: March 2024 - Due for review: August 2026