What should I do if I have fertility problems?
If you have been trying unsuccessfully for a pregnancy for 12 months, without using any form of contraception, you should contact your GP for further advice
Your GP will normally wish to review you and your partner together. During the assessment, both you and your partner need to be fully checked. Your GP may refer the male partner to see a urology specialist who looks after male fertility issues. Your female partner will be referred to see a gynaecologist. Sometimes, you might see both a urologist and a gynaecologist, as a couple, in the same clinic. Investigations of the female partner are not considered on this page.
What are the facts about male infertility?
- 1 in 7 couples in the UK are unable to have difficulties conceiving a child;
- In half (50%) of these couples, a problem may exist with the male partner;
- Even if a male factor is found, the female partner should also be ssessed;
- Urological investigation may reveal a potentially reversible underlying cause for male-factor subfertility and full assessment by a Urologist is recommended in all cases of male-factor infertility; and
- In many cases, the underlying cause cannot be identified or reversed, in which case assisted conception may offer the best chance of pregnancy;
- This may involve surgical sperm retrieval in cases where no sperm is seen in your ejaculate.
What should I expect when I visit my GP?
Your GP should work through a recommended scheme of assessment for men with infertility. This will normally include some or all of the following:
A full history
Your GP will enquire about lifestyle factors and past medical history:
- Your job;
- Work pressures;
- Exposure to excess heat (heated car seats, hot baths, steam & sauna rooms);
- History of conceiving previous children;
- Frequency of unprotected intercourse;
- Concerns with erection or ejaculation;
- Previous surgery, injury or infection of the testicle or scrotum;
- Smokling habits and alcohol intake; and
- Recreational or non-recreational drug use (e.g. anabolic steroids).
A physical examination
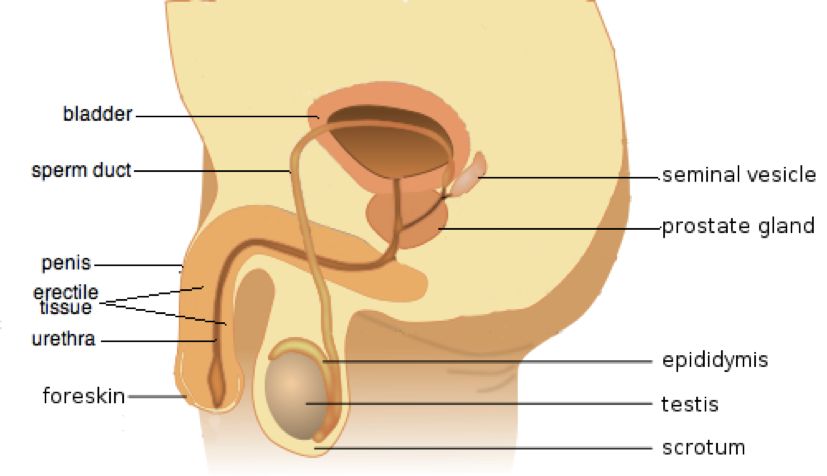
A general physical examination will be performed, paying particular attention to the genital region (your testicles and scrotal contents).
Additional tests
The usual tests performed are:
a. Semen analysis
You will need to provide at least two semen specimens for analysis. These should be done at least three months apart to check two different cycles of sperm production (each normally about 74 days). The most important levels are:
- the amount of sperm per millilitre (i.e. sperm concentration, typically more than 16 million per ml),
- the total number of sperm in the ejaculate sample (i.e. sperm count, typically more than 39 million);
- the swimming ability of the sperms (i.e. sperm motility, typically more than 30% of the sperm should be moving); and
- the number of normal-looking sperm (i.e. sperm morphology, typically more than 1-in-25, or 4%, of the sperm sample should look normal)
How to do a sperm count
b. Hormone measurements
Blood tests are done to check your levels of testosterone, prolactin, FSH (follicle-stimulating hormone), LH (luteinising hormone) and thyroid hormones. These can be used to give an indication of the nature of the underlying problem. To obtain an accuraate testosterne measurement, the blood tests should be done first thing in the morning (between 08.00 & 11.00hr) when you have had nothing to eat or drink since midnight. The blood tests are best done before you go to see a Urologist.
c. Other specific tests
Other blood tests, usually performed by specialists, may include genetic screening tests (including karyotype checks, assessment of cystic fibrosis genes and Y chromosome micro-deletions associated with infertility). If required, these will be organised when you are seen by the urologist. The results of these test can take a few weeks to months for the resutls to be finalised.
If there is a history suggestive of male genital infection, tests such as urine or semen culture will be performed. Viral screening tests, including checks for hepatitis B, C and HIV, will be done where sperm samples may need to be stored or handled by the laboratory for IVF).
Occasionally, an ultrasound of the scrotum and ultrasound of the prostate & seminal vesicles (sperm sacs) may be required.
Before you see a urologist, you should have had two semen tests and your early-morning blood tests. Please take a copy of any results with you to your appointment; this will save a considerable amount of time in investigating and managing your fertility problems
What could have caused my infertility?
In 5% of infertile men, the cause remains unexplained (this is termed "idiopathic infertility"). It may, however, still be possible for couples to conceive naturally, provided some sperms are present.
Male infertility is either due to a problem making good quality sperm, or a problem with delivery of the sperm to the outside world.
Typical causes of delivery problems can range from issues with erections or ejaculation, to physical blockages, which can occur at any step from where the sperm is made in the testicle, to its point of delivery at the tip of the penis. Some blockages can be more easily overcome, such as a previous vasectomy. Others, such as multi-level obstruction due to infections, or being born without a vas tube cannot. In cases of "obstructive" infertility, the testicle still makes sperm normally, so sperm can usually still be directly retrieved from this source.
Issues that can cause problems with how sperm are made include:
- prescribed drugs such as chemotherapy
- recreational drugs (cannabis, cocaine, anabolic steroids),
- smoking or excessive alcohol intake
- hormonal imbalances (thyroid/ prolactin)
- previous testicular infection, injury or surgery
- raised scrotal temperatures including varicoceles, regular hot baths or recent febrile illness
- genetic problems
The damage associated with some of these situations may be reversed to allow a return to normal fertility. Genetic problems cannot be reversed, but may be overcome using direct surgical sperm retrieval from the testicle, but with a lower overall chance of successfully finding sperm than in cases of obstruction.
What treatments are available for this problem?
Many couples produce a pregnancy whilst undergoing investigations or treatment for infertility but, for those who do not, a number of treatments are available
General measures
If you have poor sperm counts, you should stop smoking, reduce your alcohol intake (to around 4 units per week), avoid recreational drugs, do not use any gym supplements or whey protein shakes, and maintain a good weight and body mass index (BMI) between 19 & 25 kg/m2.
You should avoid using computers directly on your lap, do not carry your mobile phone in your trouser pocket, avoid long soaks in a hot baths or sauna/steam rooms, and do not use heated car seats because increased temperatures can affect sperm production.
Management of impaired sperm production
You should endavour to adopt a "healthy" lifestyle with a balanced diet. Fertility-specific vitamin supplements may also have some benefits.
Besides the general measures outlined above, correction of any reversible element may potentially result in a return to normal fertility. These include correction of any hormonal abnormality or treatment of infection.
Varicoceles occur in about 35% of infertile men (and in 15% of the normal male population). The treatment of clinically significan varicoceles has been shown to be associated with an improvement in sperm number and quality, and increased rate of natural and assisted conceptiion. Treatment of clinically relevant varicoceles is now advocated by both the European Association of Urology (EAU) and the American Urological Association (AUA) in their guidelines on managing male infertility.
EAU guidelines AUA guidelines

In cases where no reversible cause is present, and no sperm is present in the ejaculate, sperm may still be retrieved successfully from the testicle in approximately half (50%) of cases using microsurgical testicular sperm extraction (MicroTESE). The sperm retrived then needs to be used in assisted conception (ICSI - see below).
Management of obstruction
 Surgical bypass may be possible depending on where the level of the obstruction lies.
Surgical bypass may be possible depending on where the level of the obstruction lies.
- blockages of the vas deferens (sperm duct) – most commonly seen after vasectomy & can be overcome with a vasectomy reversal;
- blockages to the epididymis may potentially be overcome using microsurgical epididymo-vasostomy; and.
- blockages to the ejaculatory duct (at the level of the prostate) due to scars or cysts may be overcome by resecting or opening the scar/cyst
In many cases, the obstruction cannot be reversed, and direct surgical sperm retrieval (SSR) from the testes can be performed to find sperm which may then be used for assisted reproductive techniques. The choice whether to reconstruct or obtain sperm surgically depends on a number of factors, including:
- the female partner's age;
- how many children are planned;
- the time interval since vasectomy (for vasectomy reversal).
Assisted conception techniques
Intrauterine insemination (IUI)
During IUI, motile sperms are selected and injected directly through the cervix at the time of ovulation, whilst employing drug-induced ovarian stimulation in the female partner. Depending on female partners factors (such as age), pregnancy rates per IUI cycle are between 7 & 10%
In vitro fertilisation (IVF)
During in vitro fertilisation, mature eggs are collected from the ovaries of the female partner (after drug-induced ovarian stilumation) and fertilised by sperm in a laboratory. Once fertilisation has tken place, one or more of the fertilised eggs (now called embryos) are placed into the ureterus (womb) which is where the bay will develop. One full cycle of IVF takes two to three weeks.
The two methods commonly used to fertilise eggs with sperm are:
- Conventional IVF - healthy sperm and mature eggs are mixed together and kept in a controlled environment called an incubator to allow fertilisation;
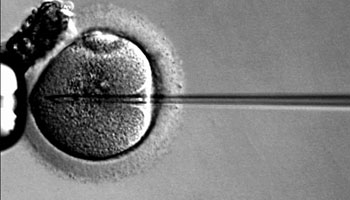
- Intracytoplasmic sperm injection (ICSI) - a single, healthy sperm is injected into each mature egg (see image below). This technique is often used when semen quality or sperm number are an issue. It may also be used if attempts at fertilisation using conventional IVF cycles have not worked.
Depending on female partner factors (such as age), pregnancy rates per IVF cycle are usually between 20 & 40%.
What options are available if no sperms can be found?
Donor insemination (DI)
Donor semen is carefully screened for infections and a donor is selected to have similar attributes to you. This is the only viable option if you have no sperms at all, and you do not have obstruction which can be relieved surgically.
Adoption
If you do not to have any success with other treatments, you may wish to consider adopting a child. Your GP, local fertility centre and local/national adoption agencies can help with this process.
Page dated: March 2024 - Due for review: August 2026