Medical Treatment of Lower Urinary Tract Symptoms (LUTS)
Recognising "at-risk" men & targeting their specific symptoms (by the Museum Staff)
From catheters, opiates & plants to a receptor-specific treatment tailored to prostate size & symptom severity
In days gone by, the prostate gland was not recognised because, in ancient medical texts, anatomical dissections were rare (and often prohibited). However, ancient Egyptian, Greek, and Roman texts do contain references to urinary difficulties in older men - symptoms we now associate with benign prostate hypertrophy (BPH) or inflammation. Physicians like Hippocrates and Galen noted the frequent need to urinate, dribbling, and pain during micturition.
Treatment during these times was largely empirical, rooted in balancing the body’s humours. Remedies included herbal concoctions, warm baths and dietary adjustments, all intended to reduce inflammation and “open the urinary passages". Opium, hemlock, and other analgesics were used to ease pain, whilst various diuretics were prescribed to aid urination. Catheterisation, albeit primitive and unsterile, was also practised to relieve acute retention.
 T
T he Renaissance ushered in a new era of anatomical & physiological study, with the first clear descriptions of the prostate gland emerging in the 16th century. Venetian anatomist Niccolò Massa (left) is credited with one of the earliest descriptions, and Andreas Vesalius (right) further advanced anatomical understanding, as well as controversially disagreeing with some of Galen's well-established anatomical findings. With clearer anatomical knowledge, physicians were able to link lower urinary tract symptoms with prostatic disease.
he Renaissance ushered in a new era of anatomical & physiological study, with the first clear descriptions of the prostate gland emerging in the 16th century. Venetian anatomist Niccolò Massa (left) is credited with one of the earliest descriptions, and Andreas Vesalius (right) further advanced anatomical understanding, as well as controversially disagreeing with some of Galen's well-established anatomical findings. With clearer anatomical knowledge, physicians were able to link lower urinary tract symptoms with prostatic disease.
Physicians recognised the different causes of urinary symptoms, such as BPH and prostatitis, although diagnostic clarity remained limited. However, the invention of the cystoscope in the late 1800s allowed direct visualisation of the bladder and urethra, thus helping in diagnosis. Ultimately, however, surgical treatment, with all its potential morbidity & mortality, was the only option available to patients for many years.
The natural history of LUTS
The first decision to be made in men with LUTS has always been whether treatment is necessary, based on urinary symptoms and routine investigations. Sporadic reports appeared in the 1970s, from small clinical trials, suggesting that the main risks for symptom progression were primarily poor urinary flow rate and hesitancy (which was associated with an increased risk of acute retention). These reports, however, were predominantly in men referred into a hospital setting.
The landmark Olmsted County Study, overseen by the Mayo Clinic, was a population-based study involving over 2,000 men who were followed up for LUTS (and other medical conditions). The study showed that the risk of requiring treatment for LUTS increased with age - from 3.3 per 1000 aged 40-49, rising to 30 per 1000 over the age of 70. The main risk factors for requiring treatment were:
- a higher symptom score on the AUA scale;
- a peak urinary flow rate <12 ml/sec;
- a prostate volume >30 ml; and
- a PSA level >1.3 ng/ml.
Together, these factors produced a four-fold increase in the risk of needing treatment. The "bottom line" was that 1 in 4 men over 70 in the study group would eventually require treatment for their symptoms and, in 1 in 10, that treatment would involve surgery.
The first, effective medical treatments
 Drugs to relieve outflow obstruction
Drugs to relieve outflow obstruction
The latter half of the 20th century saw the introduction of medications that transformed BPH management. Alpha-blockers that were used for treating hypertension (phenoxybenzamine was studied first) were found in the 1970s to help by relaxing smooth muscle in the prostate and bladder neck. As a result, terazosin, prazosin & doxazosin were commonly prescribed for troublesome LUTS. There were found to be generally effective in improving lower urinary tract symptoms (LUTS) and increasing peak urinary flow rates.
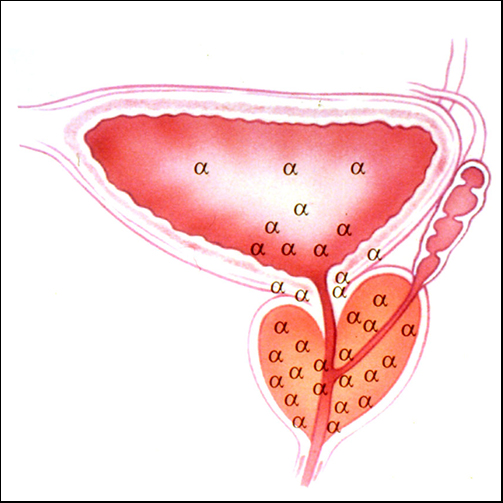
The discovery of the α1-subgroup of adrenoceptors in the bladder and prostate (pictured) resulted in the development of more LUTS-specific α1c-blockers such as Tamsulosin - now the most widely prescribed drug for prostate symptoms.
The 1990s saw the arrival of 5-α-reductase inhibitors (such as finasteride and dutasteride) which shrink the prostate by inhibiting the conversion of testosterone to dihydrotestosterone (DHT) - DHT being the main hormone responsible for prostate growth. These drugs reduced the need for surgery in many men and offered a long-term solution for moderate symptoms as well as reducing the risk of acute retention.
In the late 1980s, randomized, double-blind studies confirmed the safety and effectiveness of α-blockers (like terazosin) and 5-α-reductase inhibitors (like finasteride). Combination therapy with α-blockers and 5-α-reductase inhibitors emerged as a highly effective approach, particularly for men with larger prostates, addressing both symptomatic improvement and disease progression.
 The Veterans Affairs Cooperative Studies Benign Prostatic Hyperplasia Study, reported in 1996, was the first study to compare an α1-blocker (terazosin), a 5-α-reductase inhibitor (finasteride), and combination therapy with both drugs to placebo. Terazosin was shown to be significantly more effective in improving lower urinary tract symptoms (LUTS) and increasing peak urinary flow rates compared to placebo or finasteride. In this study, the combination arm did not prove to be superior to terazosin alone. Although the effect of terazosin on symptoms and flow rate was independent of prostate volume, finasteride-treated patients exhibited clinically relevant symptomatic improvement only in a subset of men with larger prostates. However, even in those patients, terazosin alone was more effective compared to finasteride.
The Veterans Affairs Cooperative Studies Benign Prostatic Hyperplasia Study, reported in 1996, was the first study to compare an α1-blocker (terazosin), a 5-α-reductase inhibitor (finasteride), and combination therapy with both drugs to placebo. Terazosin was shown to be significantly more effective in improving lower urinary tract symptoms (LUTS) and increasing peak urinary flow rates compared to placebo or finasteride. In this study, the combination arm did not prove to be superior to terazosin alone. Although the effect of terazosin on symptoms and flow rate was independent of prostate volume, finasteride-treated patients exhibited clinically relevant symptomatic improvement only in a subset of men with larger prostates. However, even in those patients, terazosin alone was more effective compared to finasteride.
There is, of course, a significant overlap between LUTS and erectile dysfunction, especially in older men and, as a result, phosphodiesterase-5 (PDE-5) inhibitors such as tadalafil are now being used together with the above agents to treat BPH and erectile dysfunction synergistically
Drugs to treat bladder overactivity
Anticholinergic drugs such as probanthine & oxybutynin have been used since the 1970s to address irritative storage symptoms associated with BPH and overactive bladder. Use of these drugs, however, has some unpleasant side-effects and may damp down bladder activity sufficiently to precipitate acute urinary retention (AUR).
The identification of specific beta-3-adrenoceptors in the bladder wall in the early 1990s (and cloning of the receptor itself) resulted in the development of β-3-antagonists such as mirabegron & vibegron that are effective against irritative LUTS (frequency, urgency & urge incontinence) without the significant side-effects & AUR risks of anticholinergic agents.
Phytotherapy (plant extracts)
Plant supplements are not as closely regulated as prescribed medications but they have been used to treat LUTS, baszed on the observation that some plant hormones are very similar in structure to human sex hormones (which control prostate growth).
Saw palmetto is one of the best-studied and most used supplements to treat BPH. Small studies have shown subjective improvemen, but several larger studies do not show any reduction in prostate size or any objective improvement in measurements of bladder outflow obstruction.
Other plant supplements have been used - beta-sitosterol, pygeum & rye grass extract - but their safety & quality have not been scientifically assessed, and their effects can vary significantly.
Recent additions
Experimental and clinical studies indicate that hypothalamic growth hormone-releasing hormone (GH-RH) and luteinising hormone releasing hormone (LH-RH) play a crucial role in prostate growth regulation. Prostate cells express receptors for these hypothalamic hormones, which can either stimulate hyperplasia or be blocked by antagonists to reduce prostate size & inflammation. Recent research has demonstrated that GH-RH & LH-RH antagonists not only reduce prostate volume but also exert potent anti-inflammatory effects, making them promising candidates for treating BPH (and prostatitis).
The "bottom line"
The treatment of LUTS due to BPH has, since the foundation of BAUS, involved clinicians (and their patients) in finding a balance between recommending simple conservative treatment with proven (but sometimes limited) effect, and embarking on surgery to resect or enucleate the prostate. Whilst the latter options have become dramatically safer & more effective over the years, many minimally invasive surgical treatments (MISTs) have been introduced, aimed at filling the gap between these two options.
Some older MIST options have fallen by the wayside, largely because short-term improvements were not maintained in the long-term. However, newer & more durable procedures, many of them performed in an outpatient setting & designed to preserve erectile function, are now being introduced, and are providing both patient & clinician with a wide range of simple, safe, effective treatment options for LUTS.
Whether they stand the test of time remains to be seen ...
Additional information
Click on any image below to access more detailed information about items & individuals featured above, or click here to go to the main History section of this website for more general history content:
|

Niccolò Massa
|
Andreas Vesalius
|
Olmsted County
|
|
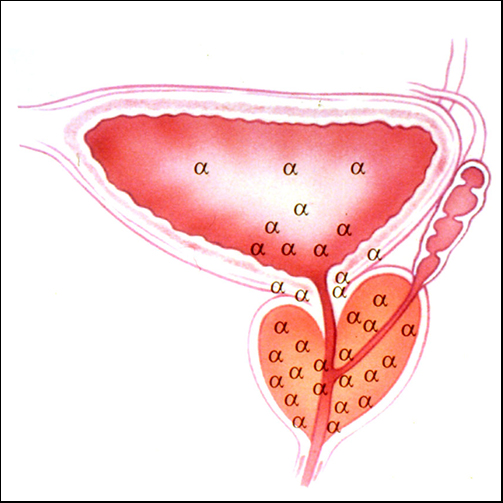
α-1-adrenergic receptor
|
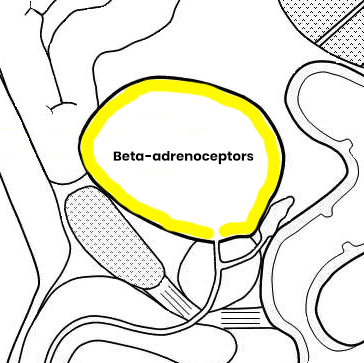
β-3-adrenergic receptor
|
|
← Back to BAUS 80th Anniversary