Advances in the Management of Erectile Dysfunction
Understanding the root causes (by the Museum Staff)
From animal extracts to gene therapy & receptor-specific treatments
Reading advertisements and watching the mainstream media today, you could be forgiven for thinking that ED was a 20th century invention, but nothing could be further from the truth. The treatment of erectile dysfunction (ED), started several thousand years ago using ancient magic/rituals together with unproven animal extracts.
In those early times, the main reason that treatment was mired in folklore, magic or unproven concoctions was the complete lack of understanding of its underlying causes. Urology has moved forwards to modern, evidence-based options such as tablet treatment, self-injection and implants, but even some of these are not recent developments.
In olden days ...
 Around 2500 BCE, the Chinese were using herbal potions & acupuncture to restore erectile capacity. Ginseng (right) was often recommended, primarily because its phallic shape was believed to encourage erections: interestingly, present evidence suggests that ginseng can be beneficial in some men with ED. Ancient Egyptian remedies involved administration of mashed crocodile hearts and blue lotus flowers: the latter do, however, contain apomorphine (a dopamine-D2 receptor agonist) now occasionally used as a second-line treatment for ED.
Around 2500 BCE, the Chinese were using herbal potions & acupuncture to restore erectile capacity. Ginseng (right) was often recommended, primarily because its phallic shape was believed to encourage erections: interestingly, present evidence suggests that ginseng can be beneficial in some men with ED. Ancient Egyptian remedies involved administration of mashed crocodile hearts and blue lotus flowers: the latter do, however, contain apomorphine (a dopamine-D2 receptor agonist) now occasionally used as a second-line treatment for ED.
The Greeks and Romans (circa 300 BCE) often used toxic, animal-based aphrodisiacs; their approach to ED made no significant contribution to scientific knowledge. It was only in the medieval Islamic world (9th to 16th centuries) that single and combined oral therapy, herbal applications, and even urethral drug delivery were employed. Their texts, however, continued to blame “demons & witches” (i.e. selected females) for causing impotence, so persecution of women was deemed an appropriate treatment!
As medicine moved forward from medieval times into the 19th century, a steadily growing body of anatomical & physiological knowledge led to the realisation that ED was primarily related to reduced blood flow in the penis. Measures to increase blood flow at this stage included various exercises, sitz baths, dietary supplements, and even electrical stimulation of the testicles. Some clinicians even recommended self-flagellation of the genitals to restore sensation and blood flow.
The early 20th century
As a bizarre aside, America in the first part of the 20th century saw the rise of Dr John R Brinkley (see link below). Brinkley had not been trained as a doctor but bought his medical degree from a diploma mill in Kansas. He became known as the "goat-gland doctor" after he achieved fame, notoriety and great wealth by transplanting goat testicles into humans to treat “sexual inadequacy” and some other conditions. He was an unashamed self-publicist and a wannabe politician with a huge, devoted following who could never be persuaded that he was a “quack”; even the eventual removal of his medical licence by the authorities in Kansas failed to quell public adulation or his self-belief. He was, however, eventually taken down by numerous cases of malpractice and wrongful death, with multiple lawsuits against him rendering him penniless and disgraced.
Timeline of advances since 1945
| 1950s |
HORMONE TREATMENT
Hormone treatment using testosterone supplements (synthetic testosterone had only just become available), was used widely in the absence of any other useful physical treatment. |
| 1960s |
PENILE PROSTHESES
Although experimental surgery to implant rib cartilage, and other rigid objects, into the penis was being performed in the 1930s, the earliest penile implants were only developed in the 1960s. They were permanently rigid and, although they allowed penetration and sexual intercourse, patients often found them uncomfortable, and levels of satisfaction were not high. |
| 1970s |
VACUUM ERECTION ASSISTANCE DEVICES
Some patients maintained good erections by using a constriction ring applied to the base of the penis, but this relied upon getting an erection in the first place. The introduction of the vacuum erection device, where an erection was “sucked” into a plastic cylinder and then a constriction ring applied to retain the erection, was a game-changer. Ejaculation was restricted in some patients, but the technique was simple and safe. The first commercial vacuum erection assistance device was developed by Dr Geddings D Osbon (see link below) |
| 1980s |
PENILE INJECTIONS & PROGRESSION TO PROSTAGLANDINS
Giles Brindley, a Cambridge physiologist ,was one of the first to demonstrate a self-administered penile injection of an alpha-blocker (phentolamine) to produce smooth muscle relaxation in the penis and, as a result, erection. For those not easily offended, the manner in which he first demonstrated this (on the podium at an international conference) can be read using the link below.
Read about Brindley's presentation
As time has moved on, papaverine and later prostaglandin-E1 (PGE-1, Alprostadil) replaced the alpha-blocker, resulting in less pain on injection, improved erections and, with PGE-1 a greatly reduced risk of priapism. Intraurethral PGE-1 was also introduced but was less effective, uncomfortable & time-consuming to administer and required the patient to use a condom because of the potential problems with ejaculating the remains of the pellet into the vagina.
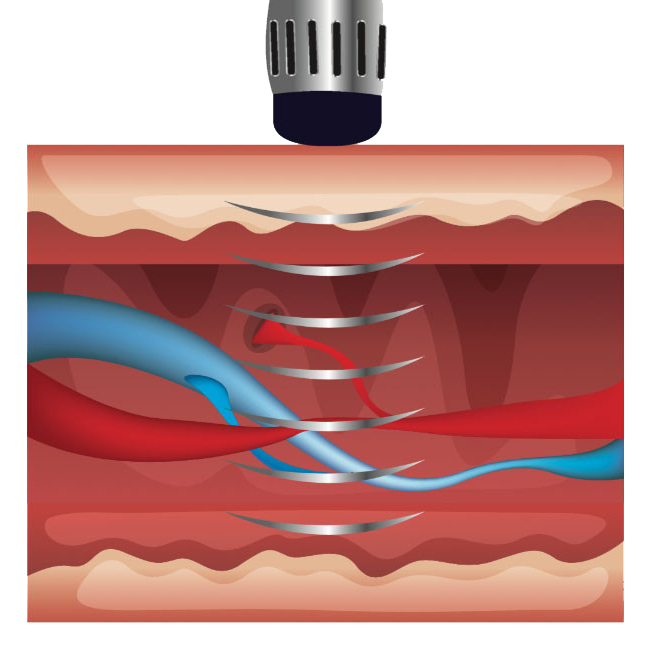
For the small proportion (less than 5%) of men with ED caused by atherosclerotic obstruction to penile blood flow, penile re-vascularisation, angioplasty or ligation of venous leaks became popular. But, as more non-invasive treatments came on the market, routine assessment of penile blood flow was no longer performed in men with ED and primary vascular intervention became less popular - reserved only for the few who did not respond to non-invasive therapy
Around the same time, the first inflatable penile prostheses, created by Brantley Scott (whose name is also associated with the earliest artificial urinmary sphincters), came on the market offering a more effective and controllable option than earlier designs. Insertion of penile prostheses has now been re-directed to a small number of large-volume, regional units with specific expertise in implant techniques. |
| 1990s & later |
UNDERSTANDING THE PHYSIOLOGY OF ERECTION
As our understanding of the physiology of erection improved, research resulted in the recognition that normal erection was the result of smooth muscle relaxation brought about by cyclic GMP (cGMP) stimulated by the release of nitric oxide (NO) within the penis. This process is inhibited by phosphodiesterase type-5 (PDE-5) resulting in deactivation of smooth muscle relaxation; PDE-5 inhibitors block the deactivation of cGMP release. thereby stimulating erection. This was was discovered accidentally while the drug was being used in a clinical trial to improve lung blood flow in patients with severe primary pulmonary hypertension.
In 1998, the first PDE-5 inhibitor, sildenafil (Viagra) appeared on the market, closely followed by tadalafil (Cialis), vardenafil (Levitra) and, more recently, avanafil (Spedra) - see link below. Initially only available on a private prescription with a Consultant's recommendation, treatment was eventually rolled out to the NHS, resulting in a seismic shift towards PDE-5 inhibitors as first-line treatment for ED of any cause. Only men with angina receiving treatment with nitrates needed to be cautious with PDE-5 inhibitors because of the risk of vasodilatation causing profound hypotension (and precipitating cardiac ischaemia). |
So, what has happened this century?
The importance of treating lifestyle factors (e.g. obesity, excessive alcohol intake, metabolic syndrome, cigarette smoking, co-existent bladder outflow obstruction) as adjuncts to the treatment of ED is now widely accepted, together with the need for supportive, psychosexual counselling in selected patients. The severity of ED and its effect on patient and partner can be assessed using symptom scoring systems (e.g. International Index of Erectile Function, IIEF; Sexual Health Inventory for Men, SHIM), and they can also help in assessing the response to treatment.
Ongoing research has now resulted in the introduction of:
- multi-drug penile injection: combinations of two, three or even four drugs are now available to patients who have a poor response to single-agent injections;
- low-intensity shockwave therapy: sometimes effective in refractory ED by stimulating the expression of vascular growth factors in the corpora cavernosa;
- androgen replacement therapy: can treat ED effectively in hypogonadal patients when used together with PDE-5 inhibitors, and may even allow the drug treatment to be withdrawn without loss of erectile function;
- stem-cell therapy: animal studies have shown that stem cells derived from mesenchyme, adipose tissue & urine are safe and effective when injected into the penis but, as yet, there is little data from human studies; and
- other drugs: e.g. Botox, cGMP activators, selective dopaminergic-D4 receptor agonists, melanocortin receptor agonists, nutraceuticals (foodstuffs), yohimbine.
The bottom line
There has been so much progress in the last 20 years, that the future for erectile dysfunction is almost impossible to predict. It is a complex disease, often associated with multiple risk factors, and effective therapy needs to be implemented according both to identifiable, causative factors and also to the requirements of the patient and his partner. Its association with cardiovascular disease, diabetes, metabolic syndrome, bladder outflow obstruction and neurological problems means that a multidisciplinary approach to management is often needed.
There is, however, more research on the horizon, perhaps leading to additional treatment options - these include:
- gene therapy;
- platelet-rich plasma (PRP) therapy: injected into the corpora cavernosa;
- stimulation of perivascular fibroblasts through membrane signalling: in animals, repetitive erectile activity results in transmembrane signalling that causes an increase in the number of perivascular fibroblasts, counteracting the effect of noradrenaline which causes vasoconstriction at rest. Ageing causes reduced numbers of fibroblasts which results in an increased risk of ED, so any intervention that increases intrapenile, perivascular fibroblast numbers may help in ED;
- external, 3-D printed, hydrogel scaffolds: and
- gene-edited stem cell injections.
Additional information
Click on any image below to access more detailed information about individual features discussed above, or click here to go to the main History section of this website for more general history content:
Giles Brindley
|

John R Brinkley
|
F Brantley Scott
|
|

Geddings Osbon's VED
|
PDE-5 inhibitors
|
Shockwave therapy
|
← Back to BAUS 80th Anniversary