Progress in the Management of Infertility
Managing male-factor infertility in the childless couple (by the Museum staff)
From hormone treatment with limited efficacy to artificial insemination, sperm retrieval & storage, assisted conception and in vitro fertilisation
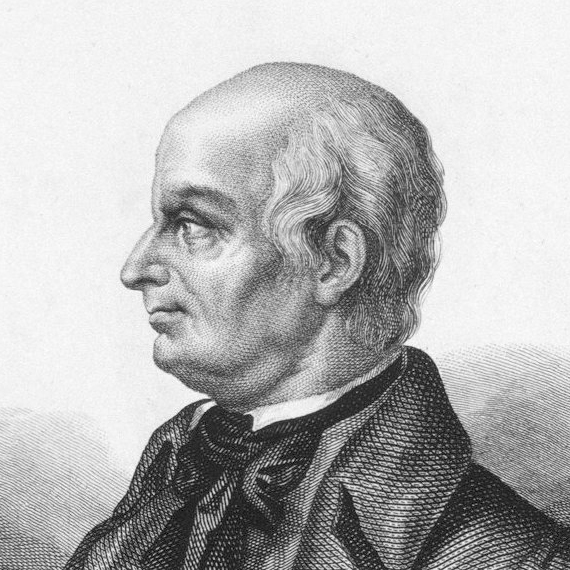
 Since ancient times, humans have wondered about the miracle of procreation; scientists and doctors studied "Generation", now referred to as embryology. In 1651, William Harvey published Exercitationes de generatione animalium following years of research on the development of the chick in the egg, the foetuses of deer and the development of insects.
Since ancient times, humans have wondered about the miracle of procreation; scientists and doctors studied "Generation", now referred to as embryology. In 1651, William Harvey published Exercitationes de generatione animalium following years of research on the development of the chick in the egg, the foetuses of deer and the development of insects.
In 1677, Antonie van Leeuwenhoek (1632 – 1723) first saw human spermatozoa with his new microscope; describing them as "animalcules" (little animals).
Artificial insemination (AI)
In 1779, Lazzaro Spallanzani, an Italian priest & physiologist, first established that an embryo develops following physical contact between egg and sperm. He also discovered a vital technique for inactivating sperms by cooling, then reactivating them later. Cryopreservation has subsequently proved to be the mainstay of most assisted-conception techniques in current use, and his work facilitated the introduction of artificial insemination (AI).
The Russian biologist Ilya Ivanov, in 1922, established AI as a practical procedure in animals but it took some time for it to be applied to humans. Assisted reproduction technology (ART) probably began with Guttmacher in 1943, who published the first report of AI in humans. For many years, it was the mainstay of ART, using frozen, donated or partner semen for men with low sperm counts, abnormal sperm morphology or impaired motility
Interestingly, it was only in the 1920s that physiologists began to understand the role of hormones (oestrogen, progesterone & gonadotrophins) in conception and reproduction, and it was not until the 1940s (coinciding with the foundation of BAUS), that synthetic hormones became available as an adjunct to other infertility treatments.
Early andrology
Once the importance of hormones had been recognised, the development of synthetic hormones flourished and, with it, the foundations of andrology as a sub-specialty were laid. These also led to hormine-induced superovulation, initially in mice but later in humans, that paved the way for egg retrieval / storage and the assisted conception techniques as we now know them.
Throughout all this, the views of female partners were rarely considered; the reasons for this were primarily cultural (and societal) at a time when the present-day concept of equality, diversity & inclusivity was not considered relevant. It would be some time before the pendulum swung to a recognition that infertility was a couple problem and that the female partner also had a right to be involved in management.
Conservative management
In the early years, men were simply advised to lose weight, stop drinking alcohol, keep their testicles cool, take more exercise and avoid stress & drug-taking, sometimes supplemented with the drug Clomiphene, an oestrogen receptor modulator which was thought to improve semen quality by stimulating hormone synthesis and spermatogenesis.
Although more than 90% of men with infertility have low sperm counts, poor sperm motility or both, and 60-70% of men with these semen abnormalities have no identifiable cause for their infertility, others do have a "treatable" cause for their infertility, In a few men, genetic or chromosomal abormalities (e.g. Klinefelter's syndrome, cystic fibrosis) or conditions such as cryptochidism could be identified but were not, of course, always treatable.
it was recognised that a small proportion of infertile males had a blockage within the seminal tract (obstructive azoospermia) or that some men were not forming any sperms at all (primary testicular failure). Conservative techniques were never going to help these unfortunate men so andrologists needed to develop other approaches.
 Obstructive azoospermia
Obstructive azoospermia
Obstruction could be diagnosed by vasography (pictured right) / ultrasound or, of course, from a past history of vasectomy. It could be treated by vasectomy reversal, epididymo-vasostomy for epidiymal obstruction due to infection or endoscopic deroofing of the obstructed seminal vesicles for ejaculatory duct obstruction; the latter could also be diagnosed by an absence of fructose in the ejaculated semen (fructose is produced exclusively in the seminal vesicles).
Some of these patients were also found to have anti-sperm antibodies, especially after vasectomy. Bill Hendry in London recognised this and successfully reduced levels of these antibodies by giving a short course of high-dose steroids to iower their levels and encourage fertilisation. The development of implanted sperm reservoirs (using autologous tissue or artificial material) seemed to be a logical step at this point, allowing sperms to be aspirated from the reservoir with a needle & syringe, but it met with limited success and never became a "mainstream" option.
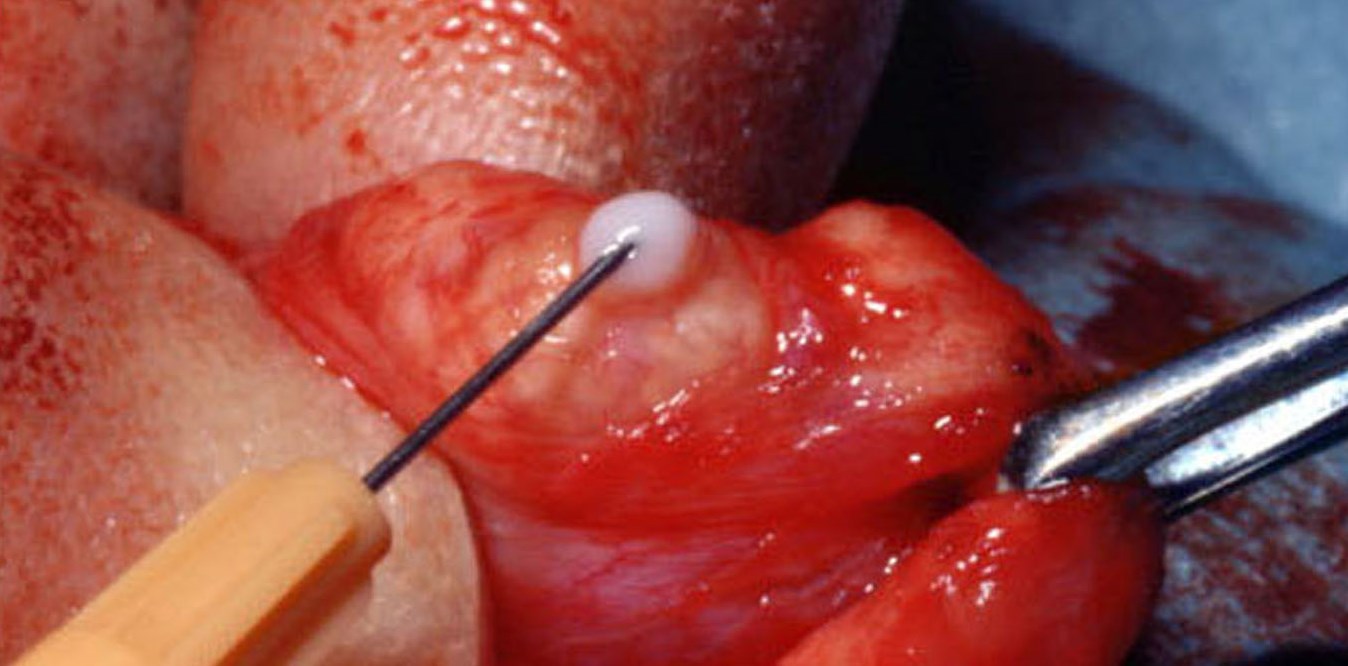 In current practice, ART with donated sperm or extraction of sperms in these men, either from the testis or epididymis (pictured below right), can also be used to allow cryopreservation and subsequent assisted conception.
In current practice, ART with donated sperm or extraction of sperms in these men, either from the testis or epididymis (pictured below right), can also be used to allow cryopreservation and subsequent assisted conception.
Primary testicular failure
The finding of grossly raised FSH levels in the blood is diagnostic of this condition. Testicular biopsy, if performed, shows no viable sperms although some abnormal forms may exist (which can sometimes be used for ICSI - see below). However, simple conservative treatment or measures for obstructive azoospermia can never help men with primary testicular failure, so assisted conception with donated sperm may be needed.
In vitro fertilisation (IVF)
Almost all infertility treatments now involve the infertile couple (not just the male partner) and employ IVF as first-line treatment. This only became a reality in the mid-20th century following the introduction of synthetic hormones and improved techniques for cryopreservation of semen (and embryos). These two advances gave clinicians the ability to control and time egg development & ovulation - the key factors that govern the success of IVF - together with the ability to perform rapid retrieval of eggs by laparoscopic or percutaneous aspiration.
IVF was first used in animals in the early 1950s, demonstrating that an embryo fertilised in a laboratory could be transferred to a womb and carried to term. In 1973, a successful human embryo transfer was reported in the Lancet from Australia but, sadly, the pregnancy miscarried after just a few days, and around 80 other attempts during the 1970s all met with the a similar fate.
| |
But, in 1978, after 10 years of rigorous study, Dr Robert Edwards1 (Lecturer in Physiology at Cambridge University), Dr Patrick Steptoe2 (Gynaecologist & expert laparoscopist in Oldham) and Jean Purdy3 (Lab technician, embryologist & nurse) changed the world for ever
|
| |
|
Louise Brown 4, the world's first IVF ("test tube") baby was born in Oldham on 28 July 1978 and infertility management was re-shaped almost overnight. Jean Purdy was, apparently, checking the fertilised ovum under her microscope just as it started its first division ,,, literally in front of her. Between them, Edwards, Steptoe & Purdy established the Bourn Hall Clinic near Cambridge as a specialist infertility centre, now a world-leading institution.
It has been estimated that, when Edwards died in 2013, more than 4 million IVF babies had been born worldwide as a direct reult of his work with Steptoe & Purdy.
Visit the Bourn Hall Clinic website
 Even though doctors had shown that IVF could be done safely & successfully, it did not become widely available for some time, partly as a result of religious, ethical & financial objections to the technique. Jean Purdy, a devout Christian herself, actively supported the introduction of IVF using vigorous rebuttals of any objections on religious or ethical grounds.
Even though doctors had shown that IVF could be done safely & successfully, it did not become widely available for some time, partly as a result of religious, ethical & financial objections to the technique. Jean Purdy, a devout Christian herself, actively supported the introduction of IVF using vigorous rebuttals of any objections on religious or ethical grounds.
Eventually, during the 1980s, increasing numbers of couples turned to IVF because it was perceived to be safe and effective, and it rapidly became "mainstream".
The Bottom Line
Clinics such as Bourn Hall now offer a range of additional options which are designed to focus clearly on equality, diversity & inclusivity:
- Treatment for single, same-sex or transgender patients;
- Intracytoplasmic sperm injection (ICSI) when sperm quality is poor (pictured above right);
- Intrauterine insemination (IUI);
- Frozen embryo transfer (FET);
- Ovulation induction;
- PGT-A (pre-natal genetic testing);
- Treatments using a donor; and
- Surrogacy.
The journey through infertility management has been a long and convoluted one, moving from ancient, largely ineffective remedies and societal judgement of women unable to bear children, to ultra-sophisticated andrological interventions that offer hope and possibilities to any couple struggling to conceive. The changes in management over the last 80 years have been massive and would have been unimaginable in 1945; where we will be even in 20 - 25 years' time is anyone's guess ...
Shortly after the death of Bob Edwards in April 2013, Louise Brown and Alastair MacDonald (the UK's first IVF baby boy) unveiled a plaque at Bourn Hall Clinic to commemorate the achievements of Edwards & Steptoe.
Click here to purchase "A MATTER OF LIFE: The Story of IVF – a Medical Breakthrough"
Additional information
Click on any image below to access more detailed information about items & individuals featured above, or click here to go to the main History section of this website for more general history content:
|

Antoine van Leeuwenhoek
|
Lazzaro Spallanzani
|
Ilya Ivanov
|
|

Patrick Steptoe
|
Robert Edwards
|

Jean Purdy
|
Footnote
1. Bob Edwards lectured undergraduates in Reproductive Physiology at Cambridge University when the former BAUS Website Editor, Nigel Bullock, was an undergraduate in the late 1960s. An excellent lecturer (not always the case with gifted academics) and a great communicator, he was eventually honoured with the Nobel Prize for Physiology or Medicine in 2010, and a knighthood in 2011. He passed away in 2013 at the age of 88.
2. Patrick Steptoe passed away in 1988 at the age of 74 from metastatic prostate cancer.
3. Jean Purdy passed away in 1985 at the tragically early age of 39 from malignant melanoma. She never received the public recognition she deserved for her contribution to the IVF programme, although Edwards & Steptoe had always acknowledged her vital role.
4. Louise Brown is now a healthy adult and has given birth to two babies of her own - both by natural means! She lectures on infertility issues and has written a book about her life.
|
← Back to BAUS 80th Anniversary