The Story of Robot-Assisted Urology
From automata via Leonardo to Da Vinci (by the Museum Staff)
 The word "robot" first appeared in 1920 as part of a stage play by the playwright Karel Čapek, from the Czech word "robota" meaning forced labour or compulsory work. In 1942, the science fiction writer Isaac Asimov was the first person to use the term "robotics". However, the earliest robots, often referred to as automata, were conceived long before this - many hundreds of years before, in fact.
The word "robot" first appeared in 1920 as part of a stage play by the playwright Karel Čapek, from the Czech word "robota" meaning forced labour or compulsory work. In 1942, the science fiction writer Isaac Asimov was the first person to use the term "robotics". However, the earliest robots, often referred to as automata, were conceived long before this - many hundreds of years before, in fact.
The development of automata (or animatronics)
Mechanical automata both of human figures and animals were created by the Ancient Chinese (circa 1000 BC) and the Greeks (450 BC), whilst a water-powered clock was described in Ptolemaic Egypt. Arab history mentions a robotic boat with automated humanoid musicians but, thereafter, little else was heard until Leonard Da Vinci (circa 1495) designed a mechanical knight, amongst many other extraordinary pieces of predictive engineering. Little was forthcoming through the Middle Ages but, with the start of the Industrial Revolution, a combination of precision mechanical engineering and the utilisation of electrical power laid the foundations of the automated machinery seen nowadays in the manufacturing industry and which, ultimately, led to the development of surgical robots.
Early robotic systems (1980s & 90s)
Surgical robotic systems only really appeared in the 1980s and 90s. They were “active” systems which operated autonomously and mechanically, without manual intervention, in response to pre-programmed instructions. They included the Arthrobot (in 1983) to assist in orthopaedic procedures, the PUMA 560 (in 1985) to guide precise needle placement during brain biopsy and ROBODOC (in 1988) to aid precise operative planning in total hip replacement.
“Probot” – the first urological robotic system
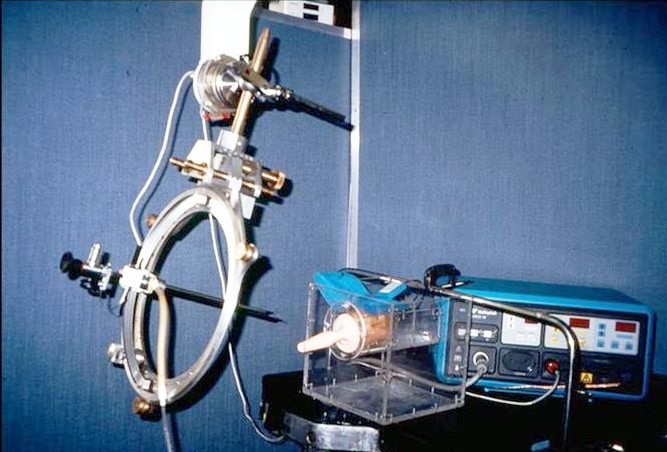 In 1989, John Wickham introduced the Probot (right), a robotic system designed in collaboration with Imperial College London to perform transurethral resection of the prostate (TURP). The robot was pre-programmed with the dimensions of the patient’s prostate, assessed with ultrasound, and it carried out the resection automatically using a rotating blade. Although it appeared successful in early trials, it did not prove commercially viable and the ultrasound reconstruction of the prostate was deemed too inaccurate for general use by urologists. Equally, additional manual intervention to coagulate intra-operative bleeding was invariably required at the end of the procedure. In 1989, John Wickham introduced the Probot (right), a robotic system designed in collaboration with Imperial College London to perform transurethral resection of the prostate (TURP). The robot was pre-programmed with the dimensions of the patient’s prostate, assessed with ultrasound, and it carried out the resection automatically using a rotating blade. Although it appeared successful in early trials, it did not prove commercially viable and the ultrasound reconstruction of the prostate was deemed too inaccurate for general use by urologists. Equally, additional manual intervention to coagulate intra-operative bleeding was invariably required at the end of the procedure.
John Wickham's work in robotics led to him sealing his place in history as "the godfather of robotics in urological surgery".
AESOP (Automated Endoscopic System for Optimal Positioning)
For the early adopters of laparoscopic surgery, the AESOP (1994) system was, basically, a robotic arm that controlled the position of the camera using voice, manual or foot-pedal commands, meaning that the image could be held steady without the need for an assistant to hold the camera. It has proved invaluable for both “non-robotic” and robotic laparoscopic procedures.
|
|
“Master-slave” systems (mid-1990s to 2010)
Early “master-slave” industrial systems, from the 1950s onwards, were based on the concept of “telepresence” - a term that describes being in one location when you are, in fact, in another. This allowed the “master” (or operator) to function safely (and remotely) in hazardous situations such as outer space, under water or inside nuclear reactors.
The major turning point for the development of surgical robotics, however, was the development of instrument systems which replicated a surgeon’s hand movements in real-time - the surgeon actively performed the procedure, but the accuracy and sensitivity of his/her movements were controlled and enhanced by the robotic system.
Intuitive Surgical created the first robotic system, the da Vinci (pictured below), based on research funded by the US military. It was originally developed for remote battlefield surgery whereby injured combatants could undergo specialist procedures by expert surgeons operating at a remote console in a different location (even on another continent). Urologists were amongst the earliest adopters of this technology, and the da Vinci system was approved specifically for prostate cancer surgery in 2001.

From 2000, robotic-assisted radical prostatectomy (RARP) for prostate cancer was largely pioneered by Mani Menon at the Vattikuti Urology Institute in America, and has rapidly became the most performed robotic urological procedure. Menon’s team have mentored countless other urologists to implement RARP in their own units, both in the USA and abroad.
Over the next 4-5 years, surgery for other urological procedures moved into the robotic-assisted age - radical cystectomy (RRC) in 2003, and partial nephrectomy (RPN) in 2004. The robotic approach has been shown to offer more accurate surgery (especially useful for preserving the erectile nerves in RARP), less blood loss, better cosmesis, reduced need for analgesics and a faster recovery than conventional open surgery with shorter hospitalisation.
Advances and expansions (2010 to present)
Since it first appeared, the da Vinci system has undergone numerous upgrades and has expanded its range of procedures. High-definition video and improved robot dexterity have improved outcomes, whilst a more streamlined design and single-port access are aimed at improving outcomes even further. Many other surgical specialties have adopted the new technology.
The range of robotic-assisted urological procedures has expanded to include simple & radical nephrectomy, adult & paediatric pyeloplasty, RPLND, ureteric reimplantation, ureterolithotomy, varicocelectomy and vasectomy reversal with more indications being added continuously.
As Intuitive Surgical’s patents have expired, newer companies have entered the robotic market (including Senhance, Versius, Hugo etc) offering improved features such as haptic feedback, open consoles, more anatomical instruments and more compact designs.
What does the future hold for robotic urology?
It is astonishing to learn that the underlying concepts of our sophisticated robotic systems, which have so dramatically improved surgical outcomes and are now used by numerous other surgical specialties, are rooted in the 18th century Industrial Revolution and in automata developed by our forefathers thousands of years ago. Urologists have played a major part in pioneering “master-slave” robotic-assisted surgery but who knows where we will be in another 80 years?
The bullet points below give some ideas, but the list is endless ...
- the use of AI to drive autonomous robots: giving greater precision and consistency, and potentially improving outcomes;
- miniaturisation / smaller systems: more agile "smart instruments" that can perform tasks lwith greater precision, reducing the need for bulky mechanical instruments; this includes robotic-assisted, single-site, laparoendoscopic surgery (R-LESS)
- use in new situations: to include many orthopaedic and emergency procedures;
- better access and cost-effectiveness: more affordable systems that could make robotic surgery accessible to a wider range of countries, hospitals and patients;
- better optics and haptic feedback: using augmented reality, dyes to highlight unseen structures and touch sensitivity;
- the use of natural orifices with flexible access: to access and operate inside the body through the vagina or colon, thereby avoiding surgical scars.
Additional information
Click on any image below to access more detailed information about individual features discussed above, or click here to go to the main History section of this website for more general history content:
|

Intuitive Surgical
|
Mani Menon
|

The Probot (& John Wickham)
|
From Leonardo to da Vinci: the history of robot-assisted surgery in urology
Yates DR, Vaessen C, Roupret M
BJUI 2011; 108: 1708-1714 |
Read the article |
Robotics in urology
McGuinness LA & Rai BP
Ann R Coll Surg Eng 2018; 100(supp 6): 45-54. |
Read the article |
The evolution of robotics in urology: the dawn of a new era
Hernal AK
Bull R Coll Surg Eng 2025; 107: 434-437. |
Read the article |
← Back to BAUS 80th Anniversary