The Management of Urinary Incontinence
From ancient moralistic misunderstandings to modern multi-factorial treatment (by the Museum Staff)
 "There are few more crippling disabilities than complete incontinence of urine. Not only does the victim suffer considerable physical inconvenience, or even misery, but there is that harder cross to bear - mental anguish."
"There are few more crippling disabilities than complete incontinence of urine. Not only does the victim suffer considerable physical inconvenience, or even misery, but there is that harder cross to bear - mental anguish."
Terence Millin, 1939
Before the 20th century, urinary incontinence (UI) presented a challenge because it was very difficult to treat medically, before the advent of surgical techniques. In women, it prevented them from fulfilling their roles as spouses and, as a result, many women were considered "impure, polluted & sexually undesirable". Rather than accelerating the search for solutions, however, this misogyny may actually have slowed that process.
Early continence devices
Urinary incontinence (UI), defined as the involuntary leakage of urine, is a condition that has affected human beings throughout history, it has carried with it significant social, psychological, and physical consequences.
With poor understanding of the complexities of the continence mechanisms in both men and women, early management was by containment (padding or rubber urinals) or compression (pessaries in women and clamps in men).

Rubber male urinals advertised in the 1913 Maw's & Co. medical instrument catalogue

.jpg) In 1826, Thomas Brown, a surgeon from Musselburgh made this ivory urethral plug (left) for a 40-year-old woman with incontinence. A small, silver stopper could be removed to allow the urine to drain. The patient was very satisfied; it allowed her to hold half an English pint of urine and, upon releasing the stopper, she was only troubled by a "slight quivering" around the neck of her bladder!
In 1826, Thomas Brown, a surgeon from Musselburgh made this ivory urethral plug (left) for a 40-year-old woman with incontinence. A small, silver stopper could be removed to allow the urine to drain. The patient was very satisfied; it allowed her to hold half an English pint of urine and, upon releasing the stopper, she was only troubled by a "slight quivering" around the neck of her bladder!
The Cunningham Penile Clamp (right) was a popular penile compression device used to prevent urinary leakage in men.
After the introduction of the new TURP operation in 1930's America, and its keen uptake by inexperienced surgeons, sales of the Cunningham lamp soared.
Vital changes in our understanding of UI
 In the past, incontinence in women was often the result of vesicovaginal fistulae caused by pressure necrosis during prolonged labour. In some parts of the world, sadly, this is still common today because of poor obstetric care. However, since the 1940s, the understanding of continence has improved dramatically, allowing more effective assessment and treatment.
In the past, incontinence in women was often the result of vesicovaginal fistulae caused by pressure necrosis during prolonged labour. In some parts of the world, sadly, this is still common today because of poor obstetric care. However, since the 1940s, the understanding of continence has improved dramatically, allowing more effective assessment and treatment.
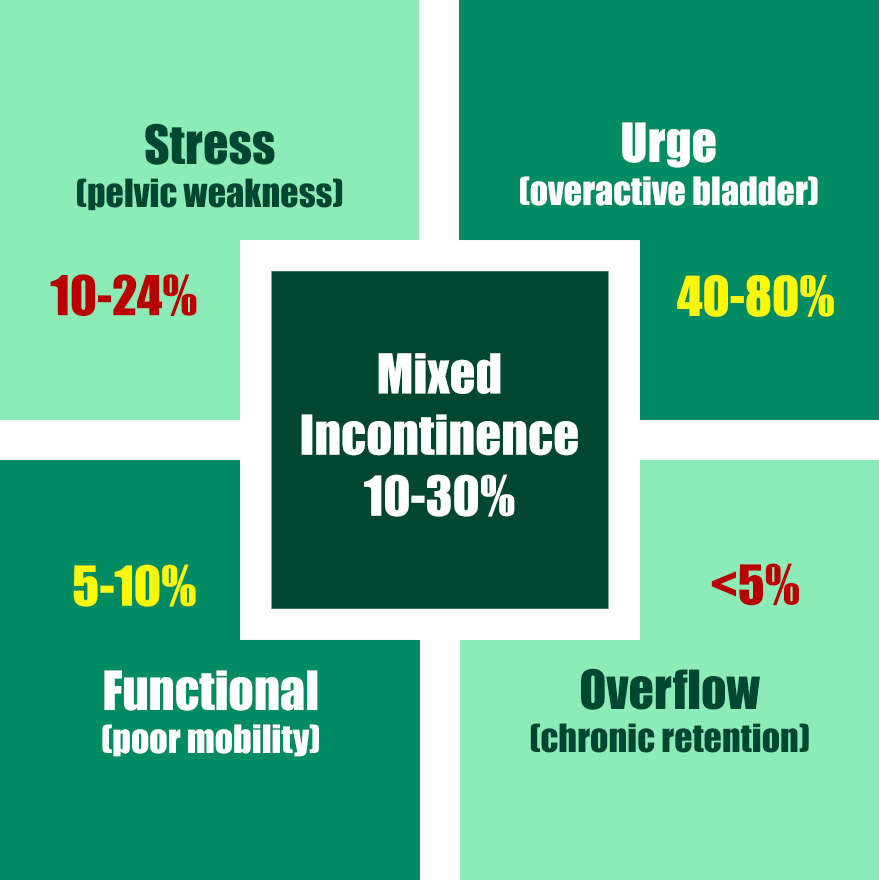
In the early 1970s, the International Continence Society (see link below) was formed and led the way on definitions and classification of UI. They divided urinary incontinence into three primary categories:
- stress incontinence (SUI)
- urge incontinence (UUI), usually due to an overactive bladder (OAB)
- mixed (stress & urge) incontinence (MUI)
Some less common categories (overflow, functional, continuous, giggle, postural & coital) have now also been included in the classification for completenss.
The SUI timeline
Form the 1940s onwards, conservative management using weight loss, regulation of fluid intake, vaginal cones, physiotherapy and pelvic floor exercises has provided first-line treatment for SUI. However, numerous physical treatment modalities have been introduced over the last 80 years, augmented by the use of oestrogen supplements (either systemic or topical).
The main therapeutic measures introduced over the last 80 years are shown below: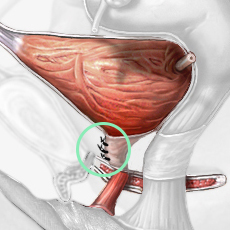
- 1930s - Urethral bulking agents: injections into the peri-urethral tissues were first introduced in the 1930s; paraffin & sodium morrhuate (1930s), PTFE (1970s), collagen (1990s) & newer agents (polyacrylamide & silicone-based agents) have all been used. Injections are easy to perform but less effective than surgery and may require repeat injections;
- 1950s - Retropubic suspensions: the Marshall-Marketti-Kranz procedure (1949) and the Burch colposuspension (1958) were the primary surgical treatments for SUI for decades. The Burch procedure (pictured right) was considered the "gold standard" before the introduction of slings;
- 1960s - Transvaginal needle suspensions: introduced in 1959, and modified by Stamey & Raz in the 1980s, these were intended to be simpler and less morbid than open retropubic procedures;
- 1970s - Artificial urinary sphincter (AUS): developed in 1977, normally used for men, but in women it is occasionally used for severe SUI that has failed to respond to the treatments above;
- 1970s - Pubo-vaginal fascial slings: autologous sling surgery started in 1978, using rectus fascia. it has proved durable in the long term with a low risk of erosion;
- 1990s - Synthetic mid-urethral slings: a major paradigm shift occurred in the 1990s with the introduction of the tension-free vaginal tape (TVT). The trans-obturator tape (TOT/TVT-O) procedure, introduced in the early 2000s, avoided the retropubic space and reduced the risk of bladder injury. Significant long-term problems caused by structural deterioration of the mesh, however, have led to its use being paused since 2018; and
- 20th century - Urinary diversion: is still occasionally used when all other forms of treatment have failed to relieve the incontinence.
The management of UUI
Poor understanding of the physiological basis of bladder function meant that, for many years, UUI was not recognised as an entity in its own right. It was only in 1881, when the physiologists Mosso & Pellacani from Turin investighatred the physiological process of bladder function and performed the first urodynamic studies, that UUI could be recognised as an important problem.
Medical treatment
Lifestyle changes such as weight loss, restricting fliud intake, bladder training, pelvic floor exercises and, more recently, percutaneous tibial nerve stimulation (PTNS) have all been used for patients with UUI.
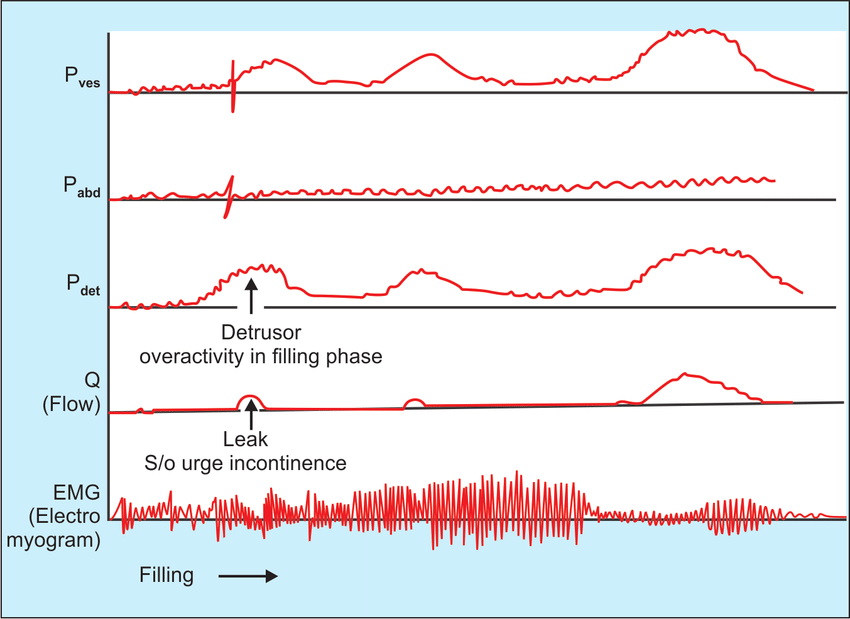 However, increasing expertise in neurophysiology recognised that cholinergic, muscarinic receptors were important in normal bladder function. From 1971 onwards, the ICS defined detrusor overactivity (DO, pictured right), overactive bladder (OAB) and urge incontinence (UUI). These factors resulted in a better understanding of neurological control of the bladder, and resulted in the introduction of anticholinergic agents.
However, increasing expertise in neurophysiology recognised that cholinergic, muscarinic receptors were important in normal bladder function. From 1971 onwards, the ICS defined detrusor overactivity (DO, pictured right), overactive bladder (OAB) and urge incontinence (UUI). These factors resulted in a better understanding of neurological control of the bladder, and resulted in the introduction of anticholinergic agents.
Non-selective anticholinergics such as impramine (1951), probanthine (1952) and oxybutynin (1975) were effective but had troublesome peripheral side-effects and caused significant drowsiness due to drug penetration of the blood-brain barrier.
Selective anticholinergics, targeting M2 and/or M3 muscarinic receptors, were introduced from the 1990s onwards - tolterodine (1998), darifenacin (2004), solifenacin (2005) and fesoterodine (2007). Trospium, also introduced in 2007, is not M2/3 selective but does not cross the blood-brain barrier, so it does not cause drowsiness.
In 2011, the discovery of beta-3-adrenoceptors in the bladder spawned a new generation of ,medications. Beta-3-adrenoreceptor activity stimulates detrusor relaxation, so agonists such as mirabegron and vibegron were found to help to relax an overactive bladder when selective anticholinergics had failed.
Surgical treatment
- 1980 - Bladder transection: both open and endoscopic transection, resulting in partial denervation of the bladder, were described in the 1980s, but were largely rendered redundant by improved, selective anticholinergics;
- 1985 - Clam enterocystoplasty: the use of a bowel patch sutured across the vault of the bladder (extending down towards the ureteric openings) rcan educe episodes of leakage but is reserved for patients in whom conservative / drug treatment has failed; it may, of course, cause metabolic problems and there are concerns about the potential for malignancy when bowel, bladder and urine come into contact;
- 1988 - Botulinum A toxin (Botox): Botox injections into the bladder wall becamee popular in the early 1990s. They are effective but often need to be repeated, and there is a risk of systemic side-effects from the toxin; and
- 20th century - Urinary diversion: is still occasionally used when all other forms of treatment have failed to relieve the incontinence.
The bottom line
A detailed understanding of bladder and pelvic floor physiology, together with the seminal work of the International Continence Society (ICS) in defining the types of incontinence, has brought about massive changes in the management of all forms of incontinence. Padding and long-term collecting ephemera have become a thing of the past - replaced by lifestyle modifications and medications, supported by patient-centred surgical interventions if conservative measures fail to produce the desired response.
Additional information
Click on any image below to access more detailed information about individual features discussed above, or click here to go to the main History section of this website for more general history content:
|

International Continence Society
|
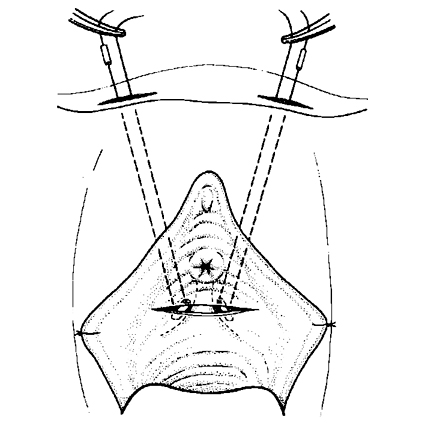
Bladder neck needle suspension
|

Mesh slings & their problems
|
← Back to BAUS 80th Anniversary